When I began research for my book on physician-assisted death, I set out to answer the question Why not? The question is not theoretical. Even a decade ago, not long after I had finished my training as a doctor specializing in intensive care medicine, serious conversations were beginning about the possibility of legalizing physician-assisted death. I realized that “where causing death was once a vice, it was soon to be a virtue”—as I shared in a previous piece for CT.
Ever since my country, Canada, legalized MAID (Medical Assistance in Dying) in 2016, I have tried to demonstrate to my colleagues and fellow citizens—beginning with, but going well beyond, my faith convictions as a Christian—that intentionally causing someone’s death contravenes and violates their incalculable worth. So long as we are committed to upholding the intrinsic value of persons—so long as we insist that their value does not merely derive from their usefulness to others or to themselves—it is inappropriate and unethical for us to seek or to offer physician-assisted death.
More than that, relying on our own sense-experience and human faculties, we cannot confidently claim to know what it is like to be dead. Therefore, it is unwise and imprudent to seek and (especially) to offer physician-assisted death. Both these reasons, I think, count quite strongly, and seem to provide a very good answer to the Why not? question.
Is the case then closed? Not quite, I think.
For to respond effectively to this issue, we must not only address the Why not? question. We must also respond to the Why? question. We must address the deep, underlying motivation for seeking or offering physician-assisted death. We must face the suffering of the sufferer, and we must have something better to offer than death.
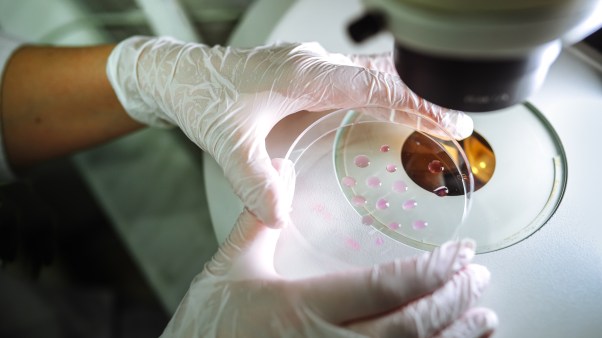
When I met Michael, he was about 30 years old. I was a young medical student, learning how to take the patient’s history and to perform a physical examination. He was the patient, admitted to the hospital for a urinary tract infection—one of many previous such admissions. Michael had primary progressive multiple sclerosis. He could barely move his arms and legs; they were stiff and contracted. He was blind.
I recall peering with my ophthalmoscope into his unseeing eyes, the white plaques of optical neuritis from multiple sclerosis effacing the surface of the retina. With the loss of some spinal cord functions, his bladder no longer contracted. To prevent urinary retention, he had an indwelling urinary catheter, but this was also a conduit for repeated infection. These infections left him much weaker even than normal—prostrate in bed, nauseated, in pain, and profoundly unwell.
As a young medical student, seeing his condition made a striking impression of suffering and disability. To that point, I had not encountered many people with such severe chronic illness. My world had been walled off from people like him. I lived with my new wife in our comfortable apartment; he lived in his nursing home. I was surrounded by friends and family; he was alone. I came and went as I pleased; he was bed-bound.
My future was that of expanding skill and opportunity. His future held out progressively increasing discomfort and limitation. In that hospital room, our worlds collided. I was the doctor-in-training; he was the lesson. But we were also just two young men struggling to find our way in the world.
Michael was shrouded in despair. He was diagnosed with multiple sclerosis as an older teenager, and the disease had progressively taken away his abilities and liberties; it had stolen everything a young man dreams of in life. Now, a decade later, he was desperately alone and desperately sad. He was deeply lonely since his disease effectively cut him off from his relationships. It was not for lack of interest on his part, although friendships under such circumstances were undoubtedly difficult.
Perhaps it was too easy for others to forget about him; perhaps it was too uncomfortable to visit. After all, we often feel threatened when we see such suffering, for we are tempted by a vague horror that the same might happen to us. Only with the kind of repeated exposure to suffering and disease that medical professionals experience during their training can one develop the disciplined sense of invulnerability necessary to cope (although this too can be profoundly unhealthy).
His loneliness was compounded by profound hopelessness. His was a progressive disease, unrelenting in its attack on his brain and spinal cord. His future held no hope for meaningful improvement, no possibility of freedom or relief. He spoke of the struggle to get through the day, feeling that there was little point in going on.
What was the purpose, the meaning, the point of such a life? It was gut-wrenching for me to sit and listen to him. I felt the cruelty and injustice of the world. Why him? Why not me? I thought.
Our clinical encounter was soon finished. I left, profoundly moved by his suffering. For a moment, I had the privilege of seeing the world through his eyes. I could sense his struggle to keep from coming apart and to retain his sense of personhood and dignity in the face of his disability and suffering. He was mourning a deep sense of loneliness, pointlessness, and hopelessness. His war for survival involved a relentless battle with despair.
This is how the desire for physician-assisted death should be understood: It is a cry of despair that cannot be ignored. To ignore that cry denies the worth of the sufferer’s life—just as much as causing their death denies their value.
Imagine for a moment that you are walking near a cliff, and you hear a cry of distress from below. Looking over the edge, you see a man clinging to a ledge, hanging precariously and desperately fearful of plunging to the rocks below.
Suppose a friend who is with you offers him a high dose of fast-acting sleeping medicine to help him fall asleep, so he no longer experiences fear or distress. You might successfully convince both your friend and the man whose life is in danger that it would be unhelpful, unwise, and inappropriate to offer or ingest the sleeping medicine. But the problem remains: How do you help the man in his moment of peril?
Likewise, even if we have successfully shown that physician-assisted death is an inappropriate and unwise way to respond to suffering, our task is not complete. We have failed to truly care for our patients if we hear their cries of despair, particularly in their requests for death, and simply throw our hands up to say, “Sorry, it’s wrong for me to end you, so I can’t help you.”
Rather, we must probe the reasons behind such a request; we must understand the fears and the pain that lead to such a cry. And we must find a way to come to their aid. It remains up to us to offer a better way for our fellow humans who find themselves in the crucible of suffering.
In many ways, an effective response to the Why? question would nullify the Why not? question. If we can show that physician-assisted death is unnecessary in the first place—if we can show how to bear the unbearable—then we might go a very long way to resolving the issue. Answering Why not? is secondary to finding a deep solution for Why?
Ultimately, when there seems to be no escape to a person’s despair, the only solution is for us to learn how to bear their suffering as the body of Christ.
Ewan C. Goligher is assistant professor of medicine and physiology at the University of Toronto.
The following excerpt is adapted with permission from Ewan C. Goligher, How Should We then Die? A Christian Response to Physician-Assisted Death (Lexham Press, 2024). Update (January 25, 2024): An earlier version of this article misstated why the author began his book research. We regret the error.
If you or someone you know needs help, call the Suicide & Crisis Lifeline at 988 or text a crisis counselor at the Crisis Text Line at 741741. In Canada, call Talk Suicide Canada at 1-833-456-4566.