All things have been created through him and for him . . . and in him all things hold together. —Colossians 1:16–17
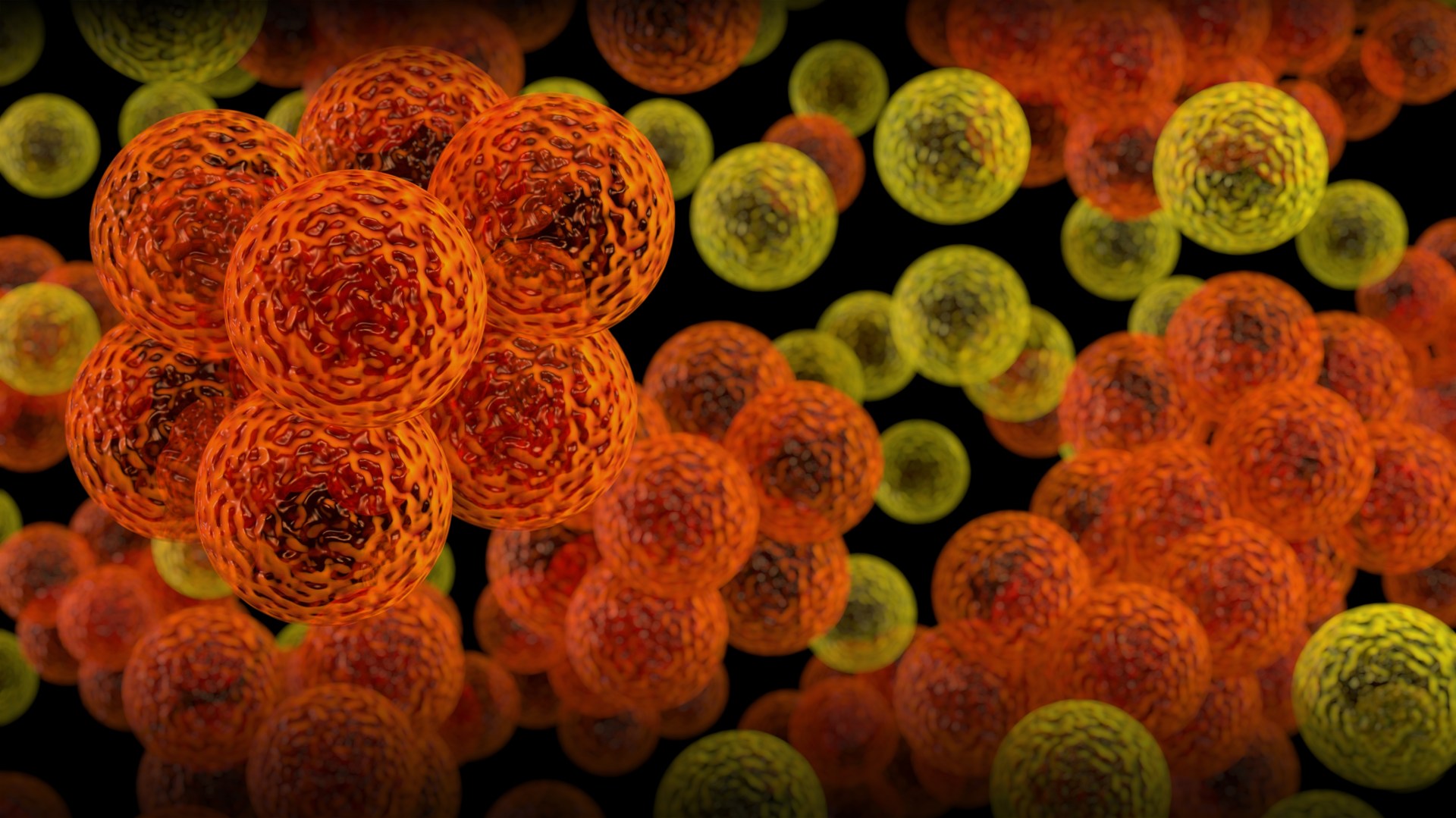
We are never alone. For the first nine months of our lives, we live inside our mother. After birth, we share our bodies with about a hundred trillion micro-organisms, even when we consider ourselves to be clean. This number is so large that micro-organisms outnumber the human cells of our bodies by about ten to one. When we die, these organisms live on to feed on our remains and on each other until there is nothing left. Some of these microbes are mere fellow-travelers, doing us neither good nor harm, but many are important to the way our bodies work.
The healthy gut contains between one and ten billion bacteria per gram of tissue. These tiny organisms perform several important tasks, [like] the bacteria [that] secrete a variety of enzymes that can digest components of food that our own enzymes cannot attack. The enzymes break down large, awkward molecules into small pieces that can be absorbed by the gut lining and by bacteria, both of which regard them as food. The bacteria consume the molecules they absorb there and then, and use the energy and raw materials to multiply and to make more enzymes. The gut lining passes the food to underlying blood vessels, from which it travels to the liver for processing and then on to the rest of the body.
Some of the food molecules attacked by bacterial enzymes would be toxins or carcinogens if left intact, so a second important function of gut bacteria is rendering food safer. They are also responsible for making some “foods,” particularly alcohol, more dangerous (in the case of alcohol, by metabolizing it to acetaldehyde, a toxic and probably carcinogenic derivative). Some gut bacteria produce significant amounts of vitamin K, which is important in blood clotting and bone growth, and which human cells cannot produce for themselves. Some also make folic acid to add to that already in food; adequate folic acid is particularly important in neural tube closure during early development.
Given their participation in digesting food, gut bacteria have plenty of access to energy and raw materials and multiply quickly. Most are, though, removed as the remains of food travel onwards: around three-fifths of the mass of a normal human stool consists of bacterial cells, many dead and some still living.
Born through Bacteria
The vagina is another environment rich in useful bacteria. Here, as in other areas potentially vulnerable to pathogens, they are needed to make the environment inhospitable for other micro-organisms that might otherwise take advantage of the warm, damp area to set up an infection. Vaginal Lactobacilli bacteria feed on components in mucus and secrete lactic acid that is too strong for most other microbes to tolerate, and also inhibit other microbes in other ways.
The vagina, in which one set of microbes helps defend against others, illustrates a general problem that also applies to the gut and to many other sites: the body has to find a way of supporting helpful bacteria while not laying itself open to invasion and attack by dangerous, pathogenic ones. Recent research suggests that humans and their helpful bacteria have, over their long association, evolved ways of communicating with each other so that the two very different types of organism can operate as a single, integrated system.
The environment in which the fetus grows, deep in the womb and surrounded by several layers of membrane, is sterile. A new human therefore forms without bacterial partners, and has to acquire them at, or shortly after, birth. Fortunately, the position of the birth canal—summarized in St. Bernard of Clairvaux’s observation, inter faeces et urinam nascimur[“we are born between feces and urine”]—is ideally suited to making sure that a baby will come into contact with bacteria from the normal human vagina, gut, urinary tract, and skin at the very moment of its somewhat messy entrance into the world. Even infants delivered by caesarean section will meet these bacteria once their mothers start to handle them, although they can take significantly longer to develop their normal bacterial flora.
When symbiotic bacteria enter the mouth of a new baby, they are swallowed along with saliva or milk and they pass through the stomach to the intestines. Here they begin their signaling dialogue with human cells.
Each part of the gut creates a nurturing environment for precisely the type of bacteria it needs. This can be illustrated by the interactions between gut cells and the species Bacteroides thetaiotamicron. Once in the digestive tract, this bacterium secretes a molecule that is detected by the lining of the small intestine. In response to that signal, intestine cells make a subtle change to their own metabolism.
Animal cells in general, including those of humans, tend to decorate the proteins they secrete or place on their surfaces with chains of sugars. Within the chains, the sugars are linked to each other with strong chemical bonds and cannot be used directly as food because the sugar-protein complex is far too large to pass through the uptake channels on the surface of a bacterial cell. The only way a bacterium can get food from these sugar chains is by having an enzyme that can cut the bonds holding the chain together, and different enzymes are needed to liberate different types of sugar from the end of a chain.
Bacteroides thetaiotamicron makes an enzyme that can liberate the sugar fucose from the ends of one of these chains. Before they receive the signal from Bacteroides thetaiotamicron, intestine cells do not place fucose residues at the ends of many of their chains but, once they receive the signal, they switch to add the fucose.
Effectively, the bacterium is saying “feed me,” and the cell is obliging—and doing so in a way that will not feed other random organisms that may be present but do not have the right enzyme to liberate fucose. Other parts of the gut express other types of linked sugars, probably in response to signals from other symbiotic bacteria. In this way, each part of the gut might create a nurturing environment for the bacterial species it needs.
Jamie A. Davies is professor of experimental anatomy at the University of Edinburgh, Scotland. This article was adapted from his book Life Unfolding: How the Human Body Creates Itself (Oxford University Press, 2014). Reprinted with permission. Scripture epigram added by the editors.